Self-Injurious Behaviours
SEPT 2021 – FEB 2022
Families and caregivers of children and youth impacted by Self Injurious Behaviours (SIB) is a 6-part educational workshop series combined with peer supports. Workshop sessions took place throughout 2021 and into 2022, and are part of a research project being conducted by the Principal Investigator (PI), Dr. Anamaria Richardson. This project aims to promote education around severe SIB, create a supportive SIB community, as well as advocate for better health outcomes.
What is Self-Injurious Behaviour (SIB)?
Self-Injurious behaviour can be defined as: self-directed injury that is non-suicidal in nature and causes physical trauma. These isolating behaviours may affect children with intellectual impairment, autism or other forms of neurodiversity. SIB is a multifaceted behaviour that is difficult to understand and treat as the diagnosis varies across individuals. Currently, proper evidence-based care does not exist, so it can be extremely challenging to care for children with severe SIB.
Are you a parent/primary caregiver of a person with Self Injurious Behaviours? Are you passionate about taking your learning to the next level? As a parent/primary caregiver do you want to learn more on how to support yourself and your child? We are bringing to you a unique 6-part series to learn and explore ways to support families and their children. These six sessions are meant to promote education around severe SIB, to create a supportive SIB community, as well as to advocate for better health outcomes.
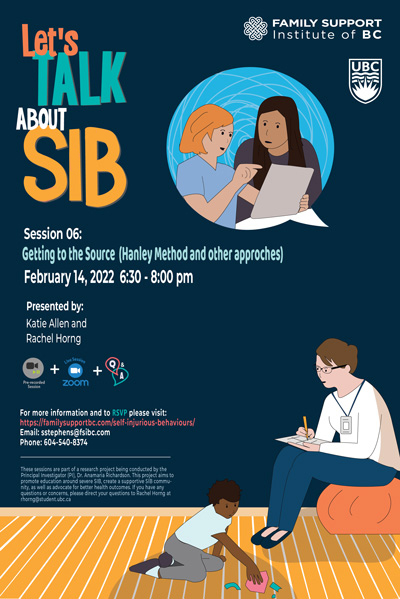
WORKSHOP SERIES: LET'S TALK ABOUT SIB
Many presentations below were created by FLEX students from the UBC Medical Program. The FLEX (Flexible Enhanced Learning) Course offers students unique opportunities to pursue a variety of scholarly activities of their interest. Natalie Cavallin (Class of 2024), Amanda Percival (Class of 2024), Matthew Tester (Class of 2024), and Allison Fong (Class of 2023) were all supervised by Dr. Anamaria Richardson (FLEX Activity Supervisor) in their FLEX projects.
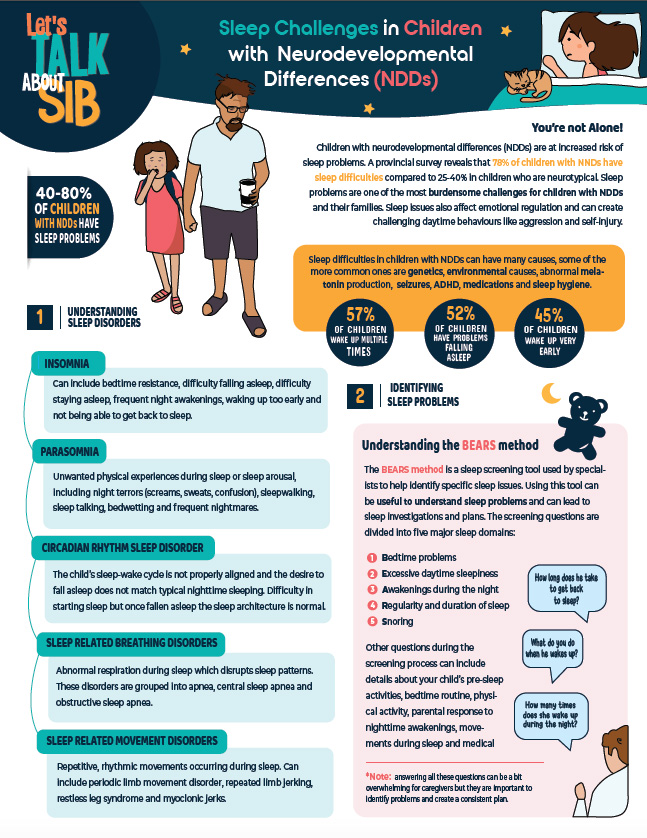
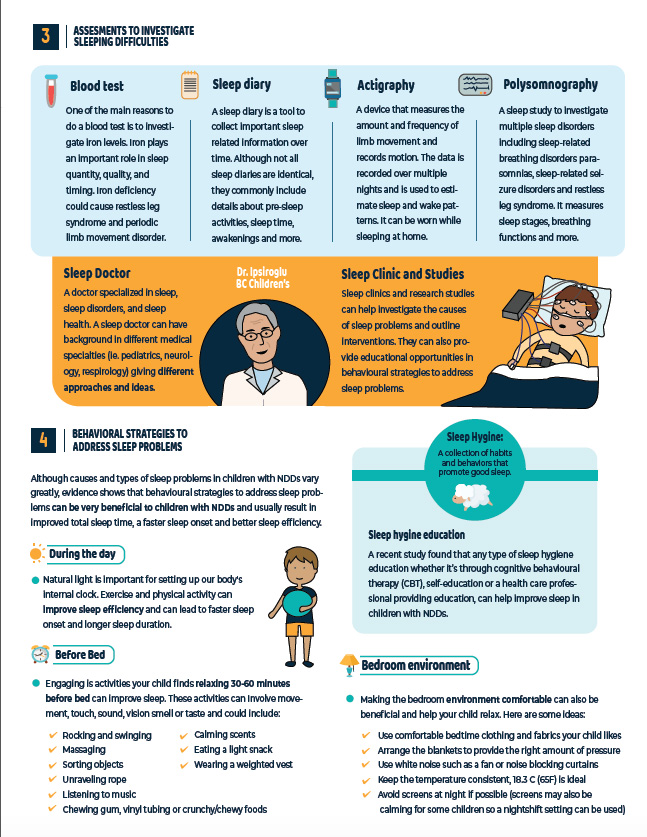
September 13, 2021 — Sleeping Like a Baby
October 18, 2021 — Safety: Equipment or Medication
November 8, 2021 — Medically Controversial Topics (Cannabis and CBD)
December 13, 2021 — A Mixed Bag: Psychiatric Comorbidities
January 10, 2022 — Things We Take for Granted: Feeding and Toileting
February 14, 2022 — Getting to the Source: Structured Behavioural Observations, Functional Analysis, Hanley Method
These sessions are part of a research project being conducted by the Principal Investigator (PI), Dr. Anamaria Richardson.
This project aims to promote education around severe SIB, create a supportive SIB community, as well as advocate for better health outcomes. If you have any questions or concerns, please direct your questions to: Rachel Horng.
REGISTRATION
1: Register Online
2: Complete Consent Form
(email to Rachel Horng)
3: Take our Pre-Session Survey
SPEAKER SESSIONS

Natalie Cavallin
Natalie Cavallin is a second year medical student at UBC. She has been working alongside Dr. Richardson and her fellow classmates on the Web-Based Parent Support Group presentation series. Natalie completed her B.Sc. (Hons) in Chemistry for the Medical Sciences at UVic where she spent five memorable years playing for the UVic Vikes women’s soccer team!
Sleeping Like a Baby
SepTEMBER 13, 2021 at 6:30 PM
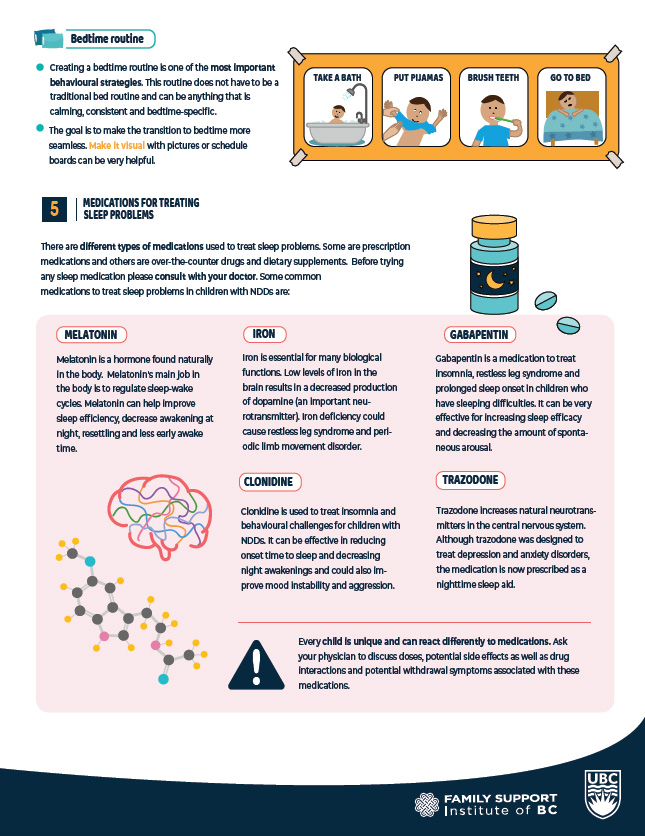
Up to 80% of children with neurodevelopmental differences have sleeping difficulties. In this talk, we will learn about the basics of sleep, common sleep challenges, assessments and treatments for sleep including behavioural strategies and medications. This session will be followed by a live 1 hour parent lead Q&A session answered by a panel of expert health care professionals.
Learning Outcomes
- To learn about the structure of sleep and why we sleep
- To learn about sleep challenges in children with NDDs
- To learn about various behavioural strategies and medications to treat sleeping difficulties

Amanda Percival
Amanda Percival is a second-year medical student at the University of British Columbia with a BSc (Hons) in cellular, anatomical and physiological sciences. Amanda worked with Dr. Anamaria Richardson, Dr. Robin Friedlander, and Katie Allen to create this presentation during her research block after finishing first year.
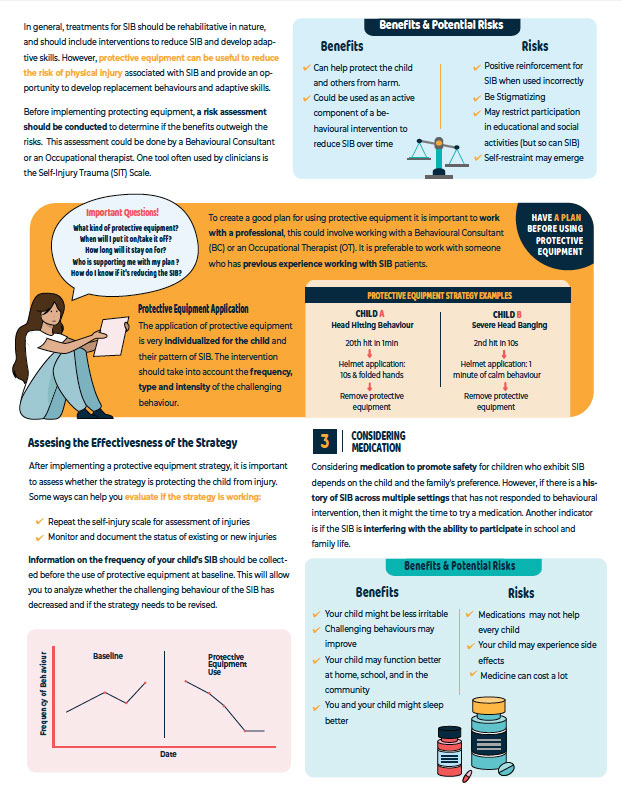
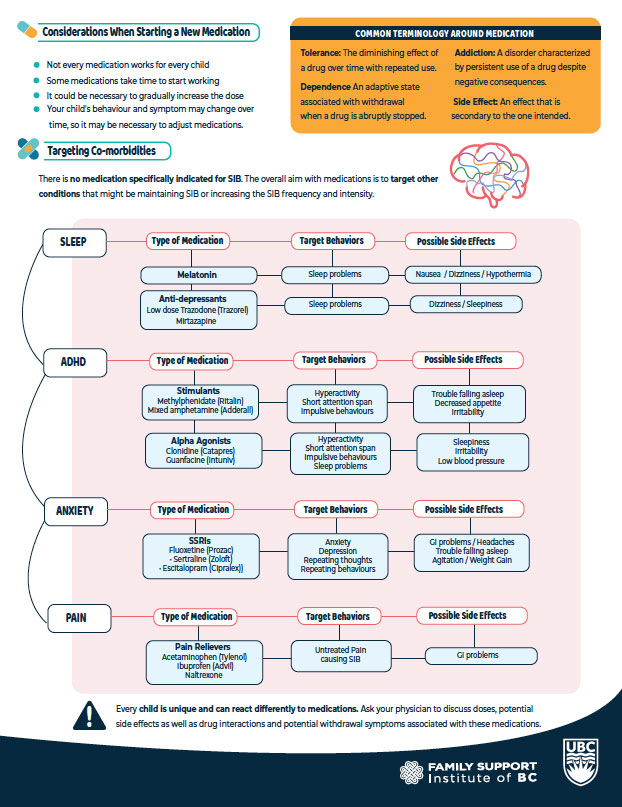
Safety: Equipment or Medication
OCTOBER 18, 2021 at 6:30 PM
Join us for a session on the use of protective equipment and medication for safety in children displaying self-injurious behaviour (SIB). We will briefly discuss the general approach to assessing and managing SIB, at what point parents might consider using protective equipment and medications, and best practices when using these safety tools.
Learning Outcomes
- Understand the general approach to SIB assessment and management
- Learn when and how protective equipment should be used for SIB
- Learn about long-term and as needed medications for SIB

Matthew Tester
Matthew Tester will be entering his second year of medical school at UBC in August of 2021. In 2019 he completed his BSc at UBC in Microbiology & Immunology with a Minor in Arts (Psychology), and worked as a research assistant at the BC Children’s Hospital Heart Centre during and after his undergrad. He loves running along the seawall and conversations over a craft pint. He had the pleasure of working with Dr. Anamaria Richardson on this presentation after completing his first year of medicine.
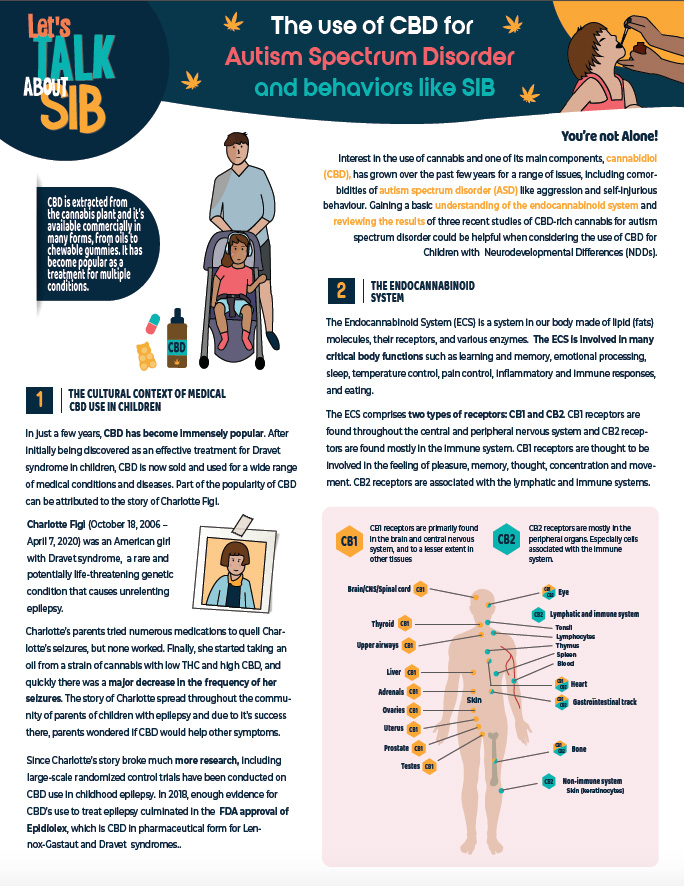
Medically Controversial Topics (Cannabis and CBD)
NOVEMBER 8, 2021 at 6:30 PM
Interest in the use of cannabis and one of its main components, cannabidiol (CBD), has grown over the past few years for a range of issues, including comorbidities of autism spectrum disorder (ASD) like aggression and self-injurious behaviour. In this talk, I will provide some context for CBD’s relatively recent rise to prominence. I give a brief background on the endocannabinoid system, as well as the components of the Cannabis plant species, namely tetrahydrocannabinol (THC) and CBD. I then discuss some of the information available online for cannabis and CBD use in ASD before digging into the wider online discourse amongst parents and caregivers. I then discuss the current state of the science surrounding the topic, focusing on three recent and prominent studies investigating CBD-rich cannabis use in treating symptoms and co-morbidities of ASD, particularly difficult behaviours. At the end of the presentation, I provide some useful resources for navigating this difficult topic.
Learning Outcomes
- Understand some of the cultural context around use of medical cannabis and CBD, especially for severe childhood epilepsy
- Gain a basic understanding of the endocannabinoid system
- Define what phytocannabinoids are and appreciate the differences between THC and CBD
- Review the methods, results, strengths, and weaknesses of three recent studies of CBD-rich cannabis for autism spectrum disorder and behaviours like SIB
- Briefly review the current trend in cannabis research in ASD
Allison Fong
Alison Fong is a third year medical student at the University of British Columbia with a BSc in Microbiology and Immunology. For the past year, she had the pleasure of working with Dr. Anamaria Richardson to prepare this presentation, and with Dr. Robin Friedlander to prepare a chart review of the patients attending the SIB Clinic at BCCH. In her spare time, she enjoys watching thought-provoking movies and writing music.
A Mixed Bag: Psychiatric Comorbidities
DECEMBER 13, 2021 at 6:30 PM
78% of children with autism have at least one mental health condition. Join us for a session in learning about common psychiatric comorbidities and their methods of treatment. We will discuss common psychotherapies and pharmacologic treatments for ADHD, anxiety disorders, OCD-related disorders, mood disorders, as well as catatonia.
Learning Outcomes
- To appreciate the prevalence of mental health conditions in children with autism and intellectual disability, and the impact they have on them and their families.
- To gain some understanding of treatment options available.
- To address some methods of complementary and alternative medicine.
Vanessa Wong
Vanessa Wong is a third year medical student at the University of British Columbia. She has been working with Dr. Anamaria Richardson, Katie Allen and her fellow classmates to give this series of Web-Based Parent Support Group presentations. She has previously completed her B.Sc. in Neuroscience at McGill University.
Things We Take for Granted: Feeding and Toileting
JanUARY 10, 2022 at 6:30 PM
Toilet training and feeding difficulties are a common issue in pediatric populations. In this session, we will dive into the importance, barriers and strategies of overcoming these difficulties. We will discuss an approach to guide parents’ plan and choice of techniques, depending on the individual child’s learning style and the context.
Learning Outcomes
- Recognize the prevalence of toileting and feeding difficulties in children with NDD
- Identify the importance and barriers of toilet training and feeding therapy
- Become familiar with the various behavioural strategies to improve toileting and feeding
Rachel Horng
Rachel Horng is a fourth-year undergraduate student working towards her BSc. in Psychology and Physiology at the University of British Columbia. She has had the pleasure of working alongside Dr. Richardson, Katie Allen, and the rest of the research team for the past year to construct this web-based presentation series.
Getting to the Source (Structured Behavioural Observation, Functional Analysis, Hanley Method)
FebRUARY 14, 2022 at 6:30 PM
In this session, we will learn about the different behavioural assessments used to treat self-injurious behaviour (SIB). We will briefly talk about how to characterize patterns of SIB through structured behavioural observation. Then we will discuss how to identify the motivators that drive SIB through a Functional Behavioural Assessment. Finally, we will learn how to control SIB through a Practical Functional
Assessment.
Learning Outcomes
- Identify the different methods of structured behavioural observation
- Recognize the components of a Functional Behavioural Assessment (FBA)
- Recognize the components of a Practical Functional Assessment (PFA)
- Differentiate between a functional analysis and an Interview Informed Synthesized Contingency Analysis (IISCA)
Q&A SESSION SPEAKERS
Katie Allen

Katie Allen, M.S., BCBA, is a master’s level Board Certified Behavior Analyst (BCBA) since 2005. Her Master of Science degree in Applied Behavior Analysis (ABA) was obtained through Northeastern University, Boston MA. Katie spent three years at the New England Center for Children, a leading day and residential program for children with autism in the United States. Upon completion of her master’s degree she spent one year working in a public school setting implementing ABA both in and out of the classroom. She moved to Vancouver in 2006 to design and implement individualized home based ABA programs for children with developmental disabilities. Her focus in training and practice has been working with individuals who exhibit severe challenging behaviour including self-injurious behaviour, aggression, and property destruction within the contexts of home, school, community and residential treatment. Katie has been active as a board member of BC-ABA for four years in the roles of President, Member at Large and Secretary. Since 2019 Katie has been working within the Provincial Health Services Authority at BC Children’s Hospital with the Self-injurious Behavior Clinic alongside a multi-disciplinary team working to assess and treat children with self-injurious behavior across the province. She has presented research at both local and international venues, and spoke on invitation to a variety of organizations including parent groups, BC Children’s Hospital, Fraser Health, and school districts. Katie uses data analysis to assess the effect of challenging behaviours on their environment, providing research opportunities to interns and staff in residential treatment facilities and private home-based intervention. Her research interests include self-injurious behavior, functional analysis, and errorless learning strategies
Dr. Dean Elbe

Dr. Dean Elbe, PharmD, BCPP is a Doctor of Pharmacy, Residency Trained and Board Certified Psychiatric Pharmacist who has worked as a clinical pharmacy specialist in Child & Adolescent Mental Health at BC Children’s Hospital since 2007. Dean is a clinical instructor in the Faculty of Pharmaceutical Sciences at the University of British Columbia (UBC), and an honorary Associate Member of the Department of Psychiatry in the UBC Faculty of Medicine.
Dean is an international speaker on Child and Adolescent Psychopharmacology and Food-Medication Interactions. He is the lead editor of the 4th edition of the Clinical Handbook of Psychotropic Drugs for Children and Adolescents, an Assistant Editor of the Psychopharmacology column of the Journal of the Canadian Academy of Child and Adolescent Psychiatry and the Project Lead on development of the DrugCocktails.ca website, a website that helps youth and professionals “get the facts” about the risks of mixing prescription medications with substances of abuse.
Robin Friedlander

Dr. Robin Friedlander has published two books, 17 peer reviewed articles, three book chapters and two semi-structured interviews. He has presented at more than one hundred conferences across Canada and internationally. He is the past Chair of the Developmental Disabilities Section of the Canadian Psychiatric Association and chairs the Planning Committee of the biennial B.C. Health and Wellbeing in Developmental Disabilities Conference in Vancouver, BC. Dr. Friedlander is the founder and director of the Neurodevelopmental Disorders Program in the Department of Psychiatry at UBC. Individuals with dual diagnosis (mental health and neurodevelopmental disorders) have historically been marginalized both within the developmental sector and in mental health. The Neurodevelopmental Disorders Program has been a leader in providing psychiatry residency training in this field.
Mary Glasgow-Brown

Mary Glasgow-Brown an occupational therapist who has been working with children from birth through teen years who live in many different parts of the province for close to ten years. These children have many different diagnoses including Autism Spectrum Disorder, FASD, ADHD, developmental delay and others.
Dr. Jane Hailey

Dr. Jane Hailey, MD, Clinical Associate Professor and Consultant Pediatrician, Faculty of Medicine, University of British Columbia, Vancouver, BC Dr. Jane Hailey is currently a Pediatrician in private practice and a Clinical Associate Professor at the University of British Columbia. Born in Toronto, she attended Stanford University in California, and the University of California at Berkeley, where she studied psychology and earned a teaching credential. After several years of teaching, she moved to England for premedical studies and then attended medical school at the University of Cambridge. After qualifying as a physician, she returned to Canada to complete her Pediatric residency at BC Children’s Hospital in Vancouver, spending her last year as Chief Resident in Pediatrics. From 1992 – 2014, she was a member of a large group practice, and worked as a Consultant Pediatrician with children of all ages – from newborns to adolescents. She now works in her solo office, where she sees patients by referral. She has been an examiner in Pediatrics for the Royal College of Physicians and Surgeons of Canada. She has written for Pediatric Notes, a North American weekly newsletter for the Pediatric community. She has also written and narrated a regular medical column on CBC AM RADIO, discussing a wide variety of topics in general medicine. In 2017, she began prescribing Medicinal Cannabis as part of her Pediatric Practice.
Erika Ono

Erika Ono is a registered social worker in the Neuropsychiatry and Self-Injurious Behaviour Clinics, at BC Children’s Hospital. She is an evaluation specialist at the Centre for Health Evaluation and Outcome Sciences, as well as a PhD candidate and sessional instructor at the University of British Columbia’s School of Social Work. Her research and clinical work focus on health equity and advocacy, addressing barriers to accessing services in the mental health care and social service systems. Her publications include “Falling through the cracks: How services gaps leave children with neurodevelopmental disorders and mental health difficulties without the care they need,” in the BC Medical Journal, co-authored by Dr. Robin Friedlander and Dr. Tamara Salih.
Dr. Caroline MacCallum

Dr. Caroline MacCallum is an internal medicine specialist with expertise in complex pain and cannabinoid medicine since 2013. She is a clinical instructor in the dept of Medicine; adjunct professor in the faculty of pharmaceutical sciences program, and associate member in the department of palliative care at the University of British Columbia. She is the medical director at Greenleaf Medical Clinic where she has assessed and developed cannabinoid treatment plans for more than 5,000 patients using legal medical cannabis approved by Health Canada over the past 6 years. She is the primary author of Practical Consideration for Medical Cannabis Administration and Dosing (European Journal of Internal Medicine in 2018), which was the first of its kind on medical cannabis dosing, and cited over 290 times. In 2021 she has published Duration of neurocognitive impairment with medical cannabis use; a scoping review (Frontiers Psychiatry), Practical strategies using medical cannabis to reduce harms associated with long term opioid use in chronic pain (Frontiers Pharmacology) and “Is medical cannabis safe for my patients?” A practical review of cannabis safety considerations (European Journal of Internal Medicine) She is the assistant editor for the upcoming Cannabinoids and Pain book by Springer (July 2021); and first author on nine chapters pertaining to cannabis pharmacovigilance including: mental health, youth, impairment, dosing, patient safety (contraindications & drug interactions), product safety, pain, and cannabis-opioid synergy, cannabis use disorder. Her work is available at www.safe-cannabis.com She is working with university research groups, provincial/national committees and stakeholders on the topics of cannabis dosing, management guidelines, clinical trials, patient registries and adverse event monitoring.
Dr. Osman Ipsiroglu

Based on his interest in adherence research, socio-cultural aspects of medicine, child development and neurology, Dr. Osman Ipsiroglu developed, in collaboration with medical anthropology and educational psychology, a comprehensive functional sleep/wake-behaviours assessment concept and began to transform physiological knowledge with questions of sleep health and management.
Dr. Annamaria Richardson

Dr. Annamaria Richardson is a community-based pediatrician who has been welcomed by the autism community — she specializes in severe autism, especially those with intellectual impairment and self injury. Previously, Dr. Richardson worked in complex care and in biochemical diseases — this has resulted in her interest in medical complexity as well. Her background includes being a teacher, so she understands the challenges experienced by kids navigating both systems — health and education. Recently, Dr. Richardson has also become a qualified specialist to do autism assessments. Her current interest and research are around advancing health outcomes and advocating for increased collaboration to support families and kids with severe autism. Finally, Dr. Richardson also works within many Indigenous communities — both rural and urban — and is currently working on a project to create an Indigenous focused healthy living web based portal.a
APPOINTMENTS WITH BCCH SIB Clinic
To book an appointment with a BCCH SIB Clinician, a referral to BCCH Mental Health is required. SIB Clinic is connected to the BCCH Neuropsychiatry Clinic, and all referrals are directed to Outpatient Psychiatry Department intake.
To refer a patient to Outpatient Psychiatry, please check the referral criteria and complete the referral form.